The Science of Trauma

It’s more than a single event. It’s what happens inside us when we don’t have the support
to process what we’ve been through.
There are Four Major Types of Trauma
Each one impacts the brain and body in different ways.
Acute Trauma
- A single overwhelming event: a car crash, assault, or natural disaster.
- Often what people typically think of as “trauma.”
- Even one incident can have lasting effects on how the brain and body
function—especially if there was no support afterward.
Chronic Trauma
- Repeated exposure to harmful situations over time—like domestic violence,
abuse, poverty, or neglect. - It slowly wears down the nervous system, making it harder to feel safe, trust others, or regulate emotions.
Complex Trauma
- Multiple or layered traumas, often starting in childhood, especially from caregivers. This includes neglect, abandonment, emotional abuse, or growing up in an unstable or unsafe home.
- It shapes the very foundation of identity, relationships, and self-worth.
Developmental Trauma

Developmental trauma happens when children don’t get what they need to feel safe, seen, and soothed.
It’s not always one big, dramatic event. It’s the quiet, ongoing absence of safety—emotionally, physically, or relationally.
For example:
- A baby left to cry alone for hours.
- A child who’s constantly shamed or ignored.
- A teen who never knows when a parent will explode or disappear.
This kind of trauma doesn’t just hurt—it shapes how the brain develops. It teaches kids: “I’m not safe. I’m not loved. I’m on my own.”
And that belief gets wired into the nervous system until someone helps them rewire it—with compassion, consistency, and trauma-informed care.
These are the kinds of trauma Kinship is built to heal.
Trauma Isn’t Always Obvious
A lot of people think:
“I wasn’t abused. My trauma doesn’t count.”
But trauma isn’t about comparison. It’s about impact.
You might have grown up with emotional neglect, instability, or fear. You might feel “fine” but still overreact to stress, shut down, or feel disconnected. You might be highly functional and still carry deep, unresolved trauma.
If anything in this section resonates—you’re not alone.
That’s why Kinship exists: to help people recognize their trauma, and begin to heal it—layer by layer.
What Is Survival Mode?
When the body senses danger—whether it’s real or simply perceived—it acts fast.
In a split second, your nervous system decides: How do I stay alive?
This is what we call survival mode. It’s not a choice. It’s biology.
It’s your body’s automatic response to threat, stress, or trauma.
And for many of us, especially those with childhood trauma, it’s a permanent setting.
We don’t dip into survival mode. We live there.
The Four Trauma Responses: Fight, Flight, Freeze, and Fawn
When your nervous system senses danger, it chooses one of these four pathways to keep you safe.
Fight
You try to take control. You get angry, loud, maybe even aggressive.
You’re not bad—you’re scared, and your body’s protecting you by fighting back.
Common signs:
- Explosive anger
- Controlling behavior
- Standing your ground at all costs
- Reacting quickly or disproportionately to threats
Flight
You try to escape. You stay busy. You run from confrontation, conflict, or even your own thoughts.
You’re not flaky—you’re protecting yourself the only way you know how: by getting away.
Common signs:
- Constant busyness
- Perfectionism Anxiety or panic attacks
- Avoidance of difficult emotions or conversations
Freeze
You shut down. You go numb. You dissociate from your body, your feelings, or the world around you.
You’re not lazy or unmotivated—you’re overwhelmed.
Common signs:
- Difficulty making decisions
- Feeling emotionally numb
- Procrastination or paralysis
- Disconnection from reality (dissociation)
Fawn
You try to please. You say yes when you mean no. You avoid conflict at all costs.
You’re not a doormat—you learned that the safest thing was to keep the peace.
Common signs:
- People-pleasing
- Over-apologizing
- Lack of boundaries
- Prioritizing others’ needs over your own
Why This Matters
Survival mode is brilliant—it helps us live through things we shouldn’t have had to endure. But it was never meant to be permanent.
When we live in survival mode too long, it changes everything.
Our relationships suffer.
Our health declines.
Our decision-making is driven by fear, not freedom.
Healing starts when we recognize:
This isn’t my personality. This is my nervous system.
And there’s a way out.
The Brain: Survival Mode Overdrive
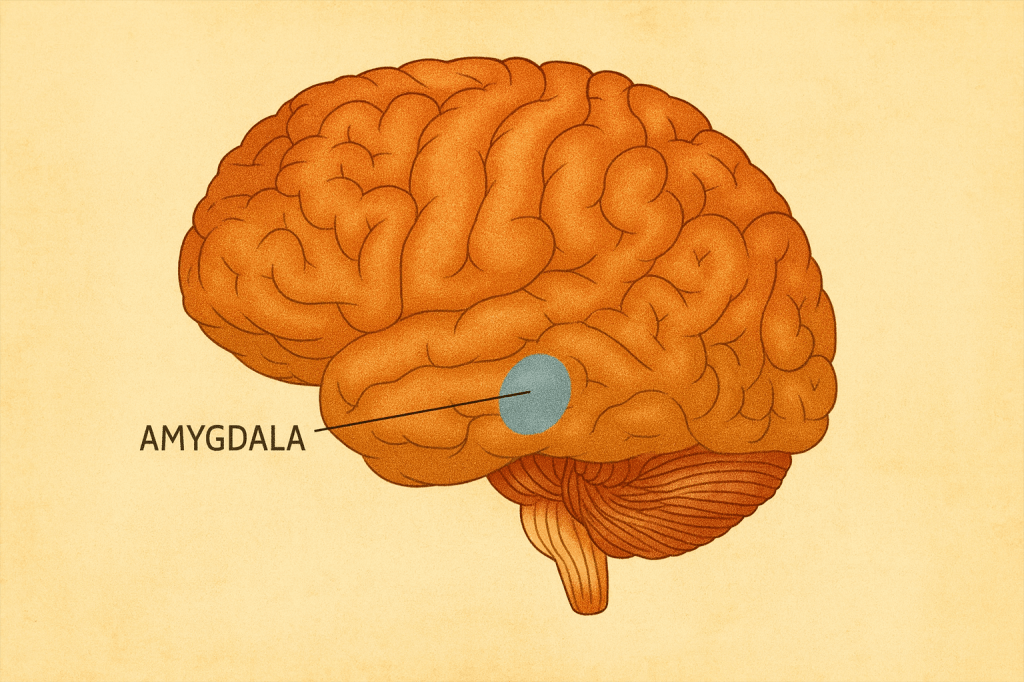
Amygdala (Fear Center): Trauma makes the amygdala hyperactive. This keeps the body in a constant state of threat detection, leading to anxiety, panic, and
hypervigilance.
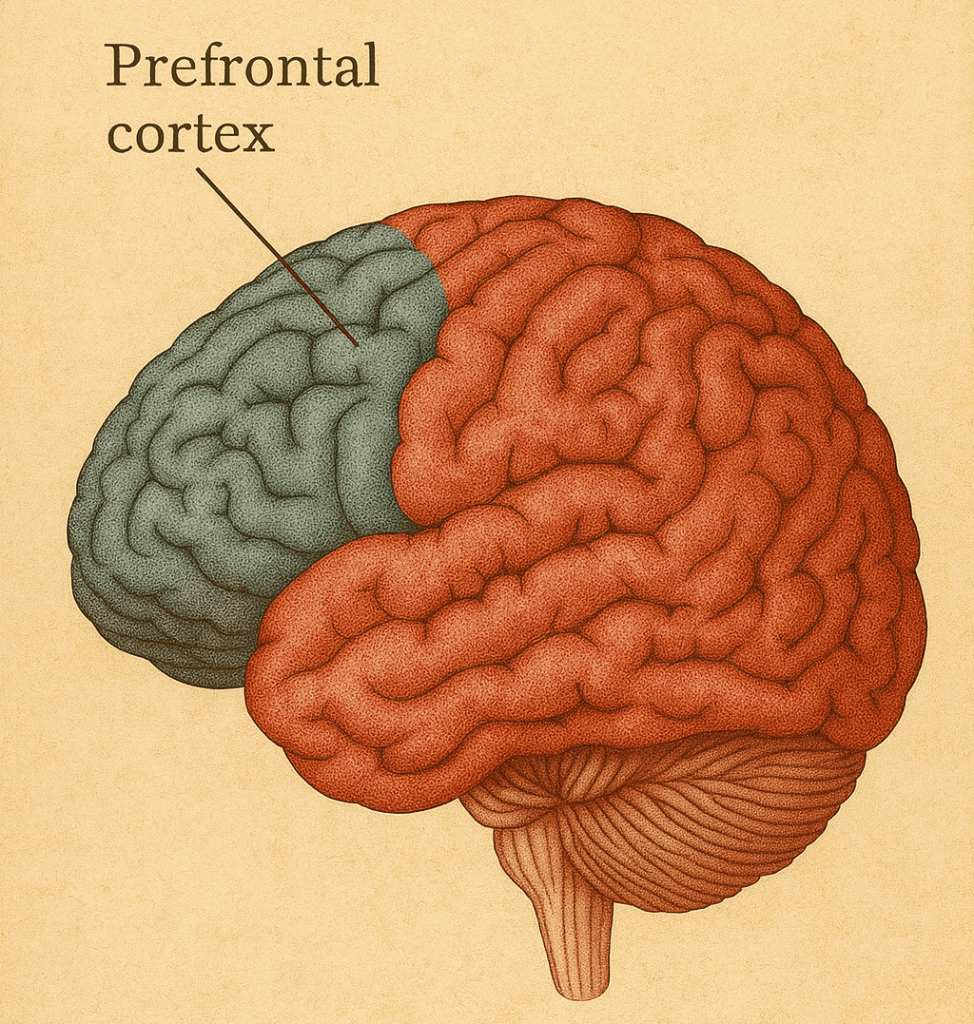
Prefrontal Cortex (Decision-Making & Logic): Trauma impairs this region,
making it hard to focus, reason, or regulate emotions. Kids with trauma are often labeled as “defiant” when they’re actually dysregulated.
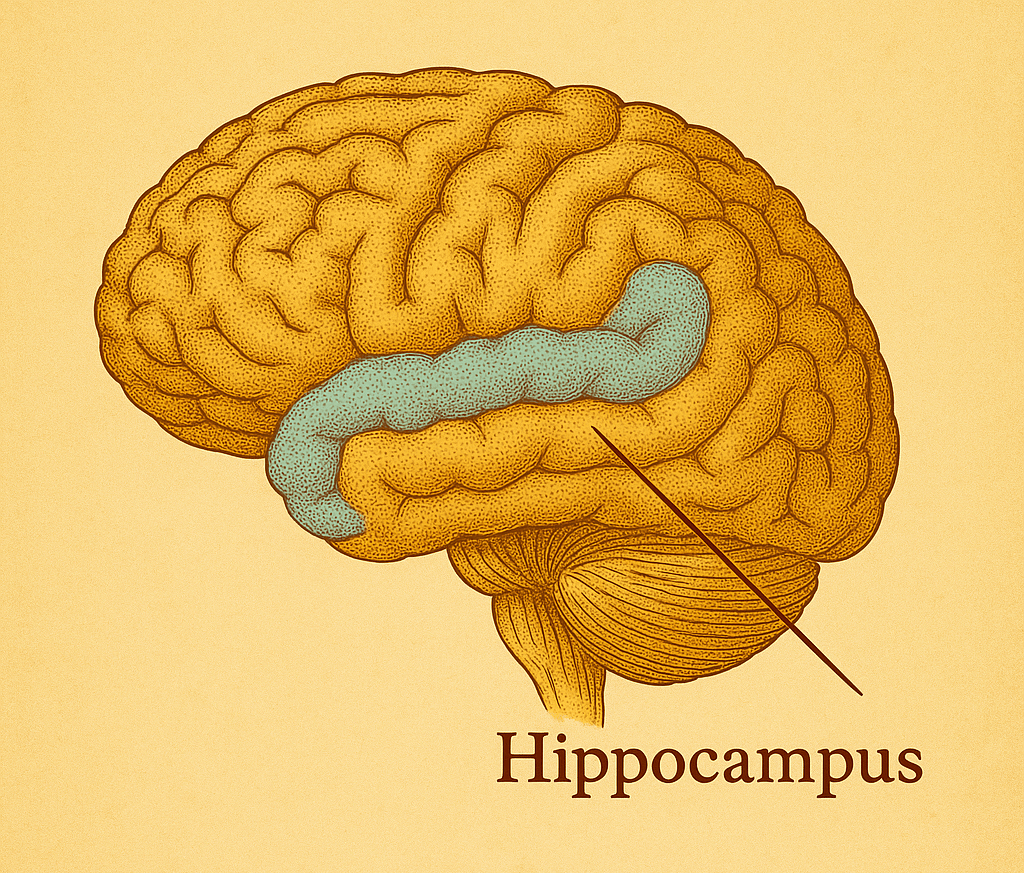
Hippocampus (Memory & Learning): Trauma shrinks the hippocampus, making it difficult to form new memories or contextualize past events. This impacts learning in school and emotional development.
Trauma-informed therapy helps calm the amygdala, restore cognitive function, and rewire the brain for trust and safety.
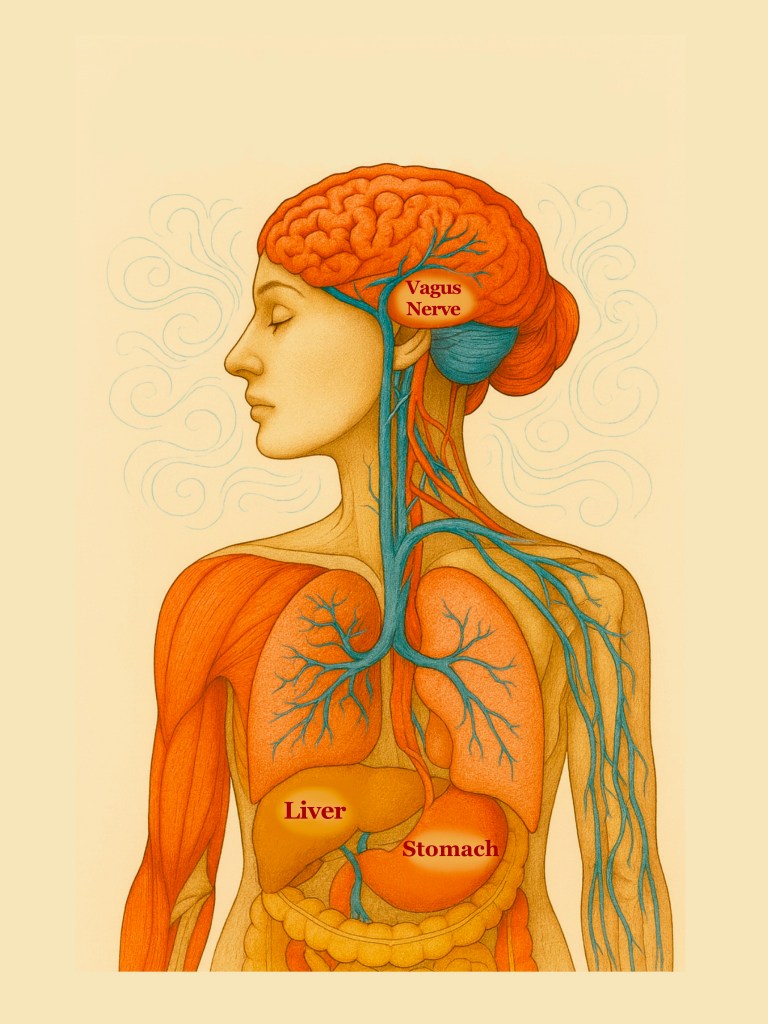
The Nervous System: Always On Alert
Sympathetic Nervous System (Fight or Flight): Trauma can lock the body into chronic stress mode—increased heart rate, shallow breathing, tension, and emotional outbursts.
Parasympathetic Nervous System (Rest & Digest): Often becomes underactive or disengaged. This makes it hard for the body to relax or feel safe.
Vagus Nerve: Central to regulating the nervous system. Trauma dulls its function, disconnecting the brain from the body’s calming responses.
Regulating the nervous system through somatic therapies, breathwork, and trauma-informed body-based care helps rebuild the ability to self-soothe.
The Endocrine System: Hormones in Crisis
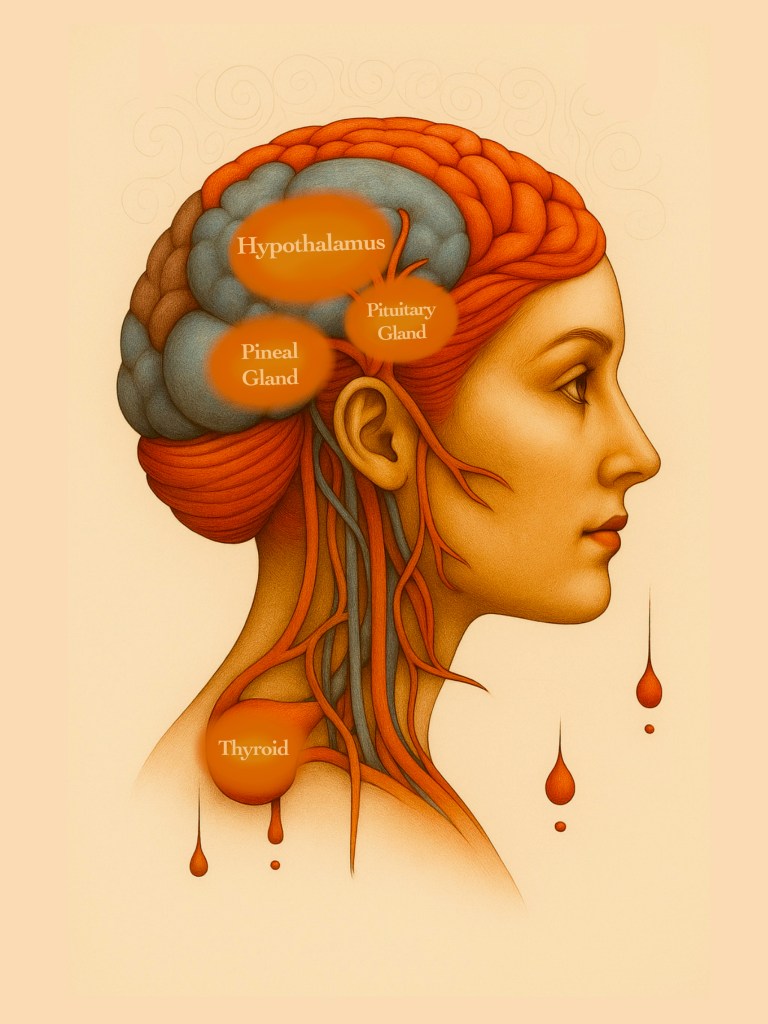
Cortisol (Stress Hormone): Chronic trauma floods the body with cortisol, weakening the immune system, increasing inflammation, and exhausting the adrenal glands.
Oxytocin (Bonding Hormone): Traumatized individuals often struggle to feel connected or safe in relationships because oxytocin levels are dysregulated.
Trauma-informed care helps rebalance hormone cycles, reduce chronic stress, and rebuild healthy attachment systems.
The Immune System: Fighting the Wrong Battles
Constant stress suppresses immunity and increases inflammation, making the body more vulnerable to illness.
Children with chronic trauma experience higher rates of autoimmune diseases, allergies, and chronic conditions later in life
Addressing trauma early can lower systemic inflammation and improve long-term physical health outcomes.
The Muscular and Skeletal Systems: Tension and Pain
Trauma lives in the body as tight shoulders, clenched jaws, migraines, and unexplained pain.
The body “remembers” even when the mind tries to forget.
Movement therapy, trauma-informed yoga, and bodywork help release stored trauma and teach the body safety again.
The Digestive System: Gut-Brain Disconnection
Trauma disrupts digestion, leading to chronic stomach issues, nausea, constipation, and IBS.
The gut is often called the “second brain.” Trauma alters gut flora and digestion, affecting mood, energy, and immune function.
Healing the gut through nutritional support and body-based therapies restores balance to the body-mind connection.
The Reproductive System: Silent Effects
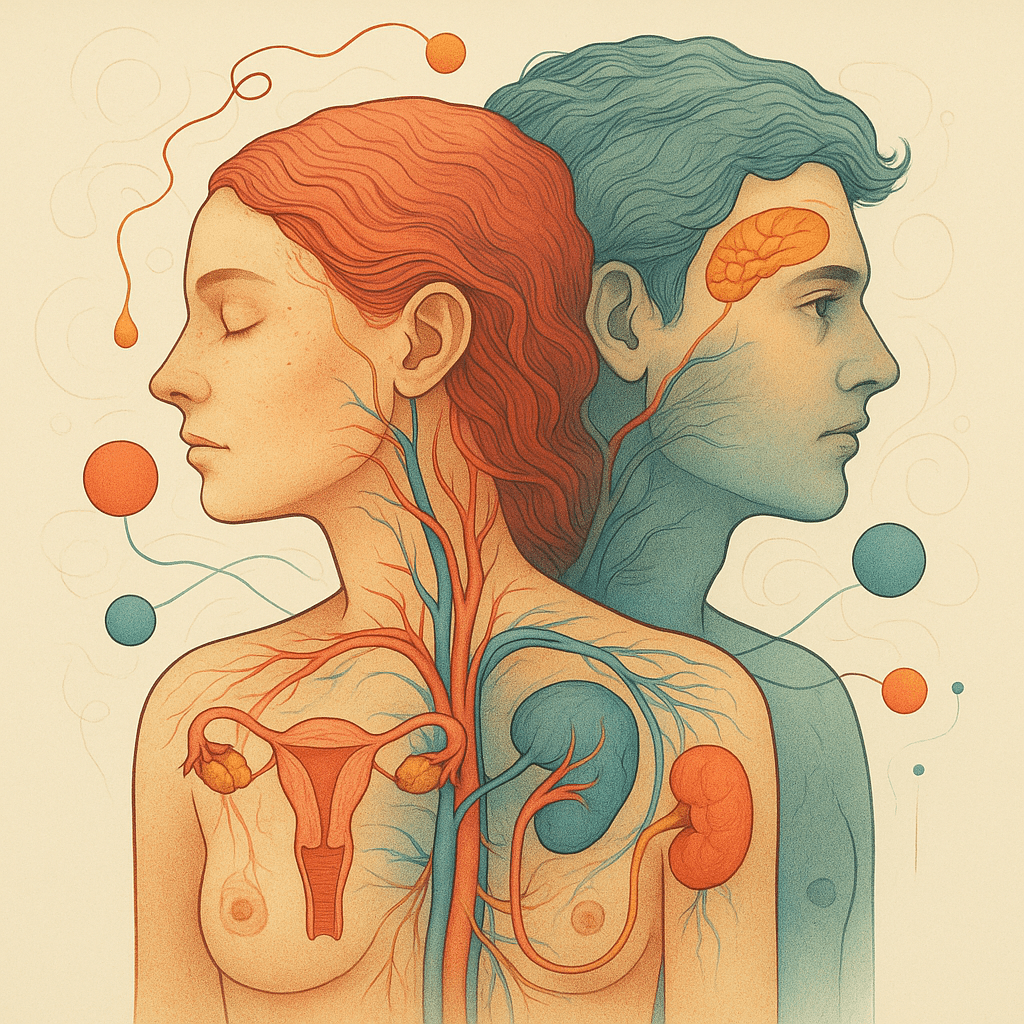
Trauma affects puberty timing, menstruation, fertility, and sexual health.
For many survivors, their body does not feel safe, which deeply impacts their relationship with intimacy and identity.
Trauma-informed therapy allows people to reclaim a sense of ownership and safety in their own body.
Conclusion: Healing Must Be Whole-Body
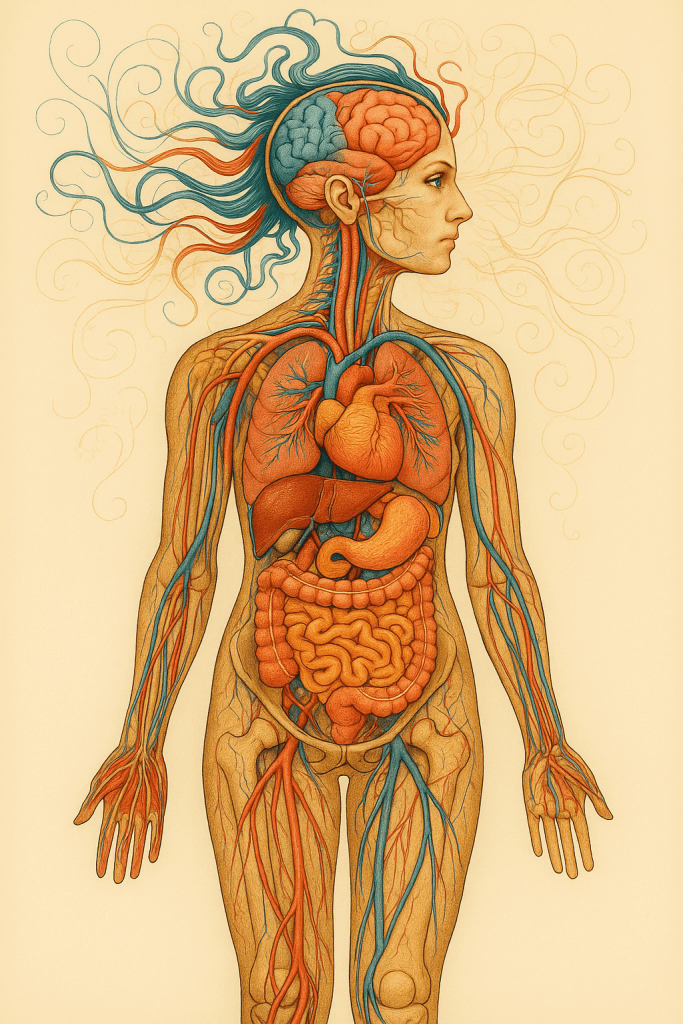
Trauma is layered.
Healing must be too.
Kinship doesn’t offer band-aids. We offer blueprints for lifelong healing—rooted in science, driven by empathy, and designed for real change.
What Are ACEs—and Why Do They Matter?
The Science Behind the Story
In the late 1990s, researchers at the CDC (Centers for Disease Control) and Kaiser Permanente made a groundbreaking discovery:
Children who experience certain types of adversity are far more likely to face serious health and emotional problems later in life. They called these experiences ACEs—Adverse Childhood Experiences.
The original ACEs study identified 10 types of trauma, such as:
- Physical, sexual, or emotional abuse
- Neglect
- Living with a parent with mental illness, substance use, or incarceration
- Domestic violence
- Divorce or separation
Each one counted as one “ACE. The higher a person’s ACE score, the more likely they were to experience:
- Mental illness
- Addiction
- Chronic disease
- Relationship problems
- Job instability
- Early death
And here’s what shocked the researchers:
The effects of childhood trauma weren’t just emotional—they were biological.
ACEs actually rewire the brain, disrupt hormones, and weaken the immune system. Trauma leaves a footprint in the body.
ACEs by the Numbers
61% of adults report at least one ACE.
1 in 6 have four or more—putting them at the highest risk for poor health
outcomes.
A child with 4 or more ACEs is:
- 12x more likely to attempt suicide
- 7x more likely to become addicted
- 4x more likely to experience chronic illness
Why This Matters for Kinship
Most of the children entering foster care already carry multiple ACEs—and the system too often adds more.
Instead of helping children heal, the current system:
- Separates siblings
- Bounces kids from home to home
- Multiple caseworkers
- Provides inconsistent therapy (or none at all)
Kinship is built to change that.
It’s not about managing trauma. It’s about healing it—through stability, safety, and trauma-informed care that works.
ACEs Are Not Destiny
A high ACE score doesn’t mean a person is broken. It means they’ve survived a lot—and healing is possible with the right support.
Science shows that protective relationships, community connection, and trauma-informed care can reverse the damage and build resilience.
That’s why Kinship matters.
Because kids shouldn’t just survive childhood—they should thrive in it.
Curious about your ACE score?
Take the original Adverse Childhood Experiences (ACEs) questionnaire here:
(You’ll be directed to an external site provided by ACEs Aware.)
My ACE Score Is 10—and I’m Still Standing

This isn’t the kind of questionnaire you want to get a perfect score on.
But I did.
I answered “yes” to every single one of the Adverse Childhood Experience (ACE) questions.
All ten.
That means I grew up with:
- Abuse
- Neglect
- A parent with severe mental illness
- Substance use in the home
- Extreme instability (housing, clothing, proverty)
- Domestic violence
- Incarceration
And more… And yet—I’m still standing.
It didn’t come easy.
I’ve spent years in counseling.
I’ve learned to set boundaries.
I’ve worked hard to understand what happened to me and how it shaped me.
But here’s what no one told me—not one therapist, not one doctor:
“Cindi, your nervous system is still stuck in survival. You need to heal that too.”
That was the missing piece.
It’s what kept me in an abusive and neglectful marriage.
It’s what kept me making decisions I knew weren’t right—because while my mind and heart were learning, my body was still trapped in fear, survival mode.
And here’s what hurts the most:
My story is not just mine.

I have siblings who also score a 10 on the ACE questionnaire.
Some of them struggled even more—with addiction, homelessness, incarceration.
My family is the statistic. But that’s why I’m here. That’s why I built Kinship.
Because we don’t just need more programs—we need to change the system.
We need to help people heal not just their minds, but their bodies, their spirits, their lives.
What If My Family Had Been Given Trauma-Informed Care?
Had my family been offered trauma-informed care, we wouldn’t just have survived.
We would have healed—years ago.
I am the only one in my family who has gone through complete, full healing.
Not because I’m stronger. Not because I’m more determined.
But because I somehow found the tools—and pieced them together myself.
It took decades.
The rest of my family?
They’re still struggling. Still living in survival mode.
Not because they don’t want to heal—but because they’ve never been shown how.
They’ve never been told that their nervous system is stuck. They’ve never been offered real, trauma-informed care. And unless you already know what to look for—it’s almost impossible to find.
We would never do this to a cancer patient.
We would never expect them to diagnose themselves, navigate treatment alone, and figure it all out in isolation.
And yet that’s what we do to trauma survivors every day.
That should be unacceptable.
Kinship exists to change that.
To bring healing out of the shadows.
To make trauma-informed care the standard, not the exception.
Because families like mine—and like yours—deserve better.
Subscribe to The Kinship Initiative Newsletter
