There Is No Real Mental Health Infrastructure—And We’re All Paying the Price.
We don’t have a real mental health infrastructure in this country. What we have is a disjointed collection of services—programs and agencies with no shared framework, no standardization, no centralized follow-through, and no real continuity of care. It’s a patchwork held together by paperwork, not people.
This is not an oversight. It’s the result of decades of avoidance, underfunding, and denial. Mental illness has always been treated as a secondary concern. We talk about the need for awareness, but we’ve built nothing underneath that awareness to catch people when they fall. We haven’t built a system that’s actually designed to help people stay in care, heal over time, or be supported long term.
What we have are silos. What we have are waitlists. What we have are trauma survivors being retraumatized by the very systems meant to help them.
And it’s happening every day.
People are forced to repeat their trauma histories over and over again because no one is holding the full story. People are being passed from one agency to the next with no continuity of care, no coordinated approach, and no trauma-informed infrastructure to hold them through the process.
This is not theoretical. It’s not even rare.
A woman in my own neighborhood recently told me that after finally gathering the courage to seek help for her PTSD, the therapist she was seeing left the agency. Just like that, she was forced to start over. It wasn’t the first time it had happened to her—and each time, the impact was just as devastating. She said to me, “I can’t keep doing this. Every time I finally feel safe enough to open up, they’re gone. And then I’m back at zero.”
She’s not alone.
Every time a provider leaves without a transition plan… Every time someone has to start over from scratch… Every time the story has to be re-told just to access care…
That is systemic retraumatization.
We would never tolerate this level of chaos in cancer treatment. If someone is diagnosed with cancer, we build an entire care plan around them. We rally family, community, and professionals. We schedule follow-ups, transportation, support groups, case coordination, and caregiver support.
But when someone is struggling with mental illness? They’re often expected to handle everything themselves—even when the very organ required to make decisions and access resources is the one that’s injured. They are asked to advocate for themselves while in crisis. They are blamed for not “following through” or “complying” with treatment, when what’s really happening is this: there is no structure designed to help them stay.
Mental illness is not a character flaw. It is not a failure of effort. It is a medical condition—one that deserves a real response.
This is exactly why the Kinship Initiative exists.
We are building a standardized trauma-informed infrastructure—a model that prevents retraumatization by design, not by luck. At the center of this model are HOPE Coordinators, who stay with each child and family from start to finish. They are the constant. The anchor. The one person who never disappears mid-treatment, mid-crisis, or mid-plan.
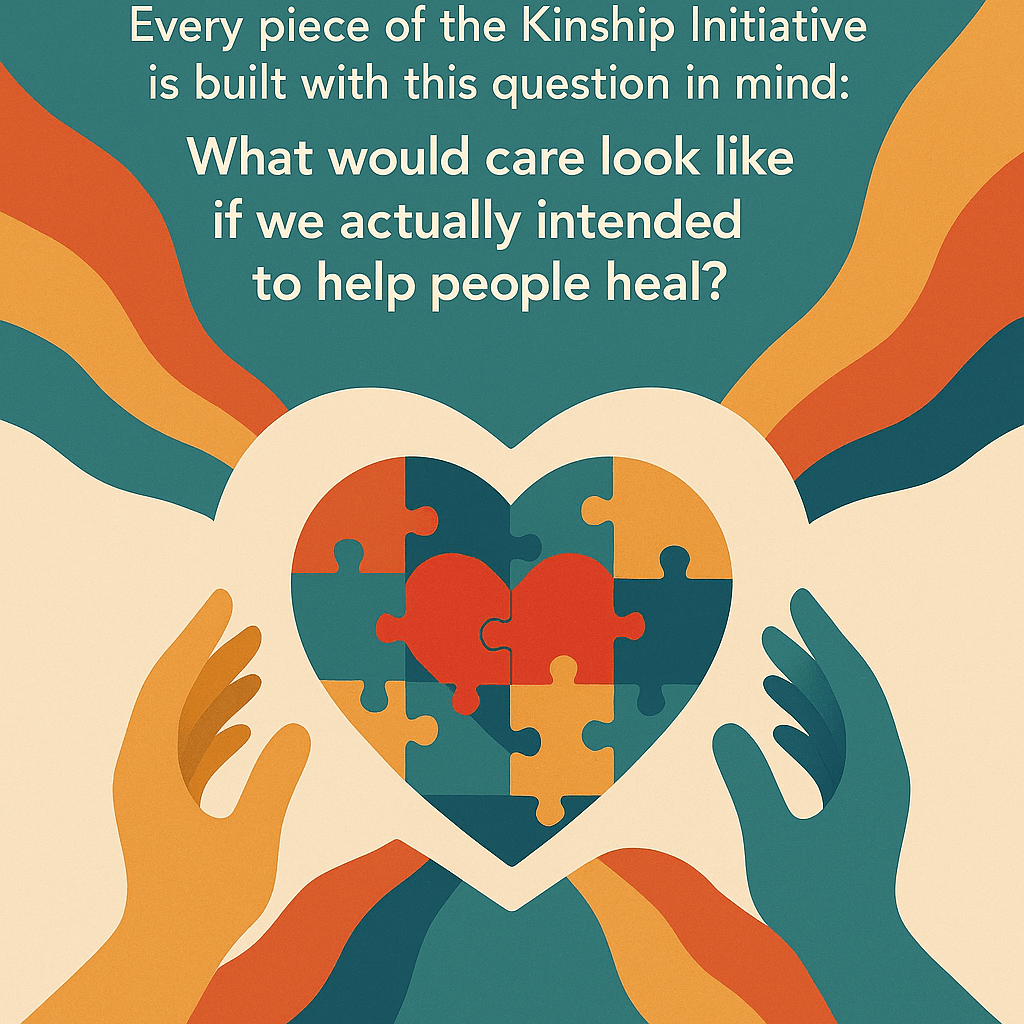
It would look like:
- Long-term relationships, not short-term interventions.
- Whole-family support, not just child-by-child management.
- Stability and safety, not just survival.
- Healing-centered policies, not just compliance checklists.
Because trauma-informed care isn’t a buzzword. It’s a blueprint. It’s the difference between someone falling through the cracks and someone finally being seen, held, and supported long enough to heal.
Right now, we don’t have that in this country.
But we’re building it. Room by room, story by story, relationship by relationship.
And we hope you’ll join us.
Subscribe to The Kinship Initiative Newsletter
